Summary:
Long wait times, delays in diagnosis, and inconsistent information about endometriosis in videos, websites, or social media posts can affect your understanding of endometriosis. Myths like the idea that hormones are dangerous, surgery is the only treatment, or pregnancy is a cure can stop people from exploring safe and effective options like hormone therapy. It’s important to check all info for accuracy, ask your doctor if it applies to you, and get referred to a specialist right away.
Demystifying Myths for Endometriosis Treatment
Getting diagnosed with endometriosis in Canada can be challenging. Wait times for specialists are high in most provinces, and exploratory surgery is still the best way to confirm you have it. Unfortunately, this means it often takes five years or more for patients to get real answers or relief from their symptoms.
Delays and problems accessing care are a big part of the reason why so many people turn to social media influencers and other online websites when they want to learn about endometriosis. Third-party educators like these are not reliable sources of information on endometriosis or how to treat it.
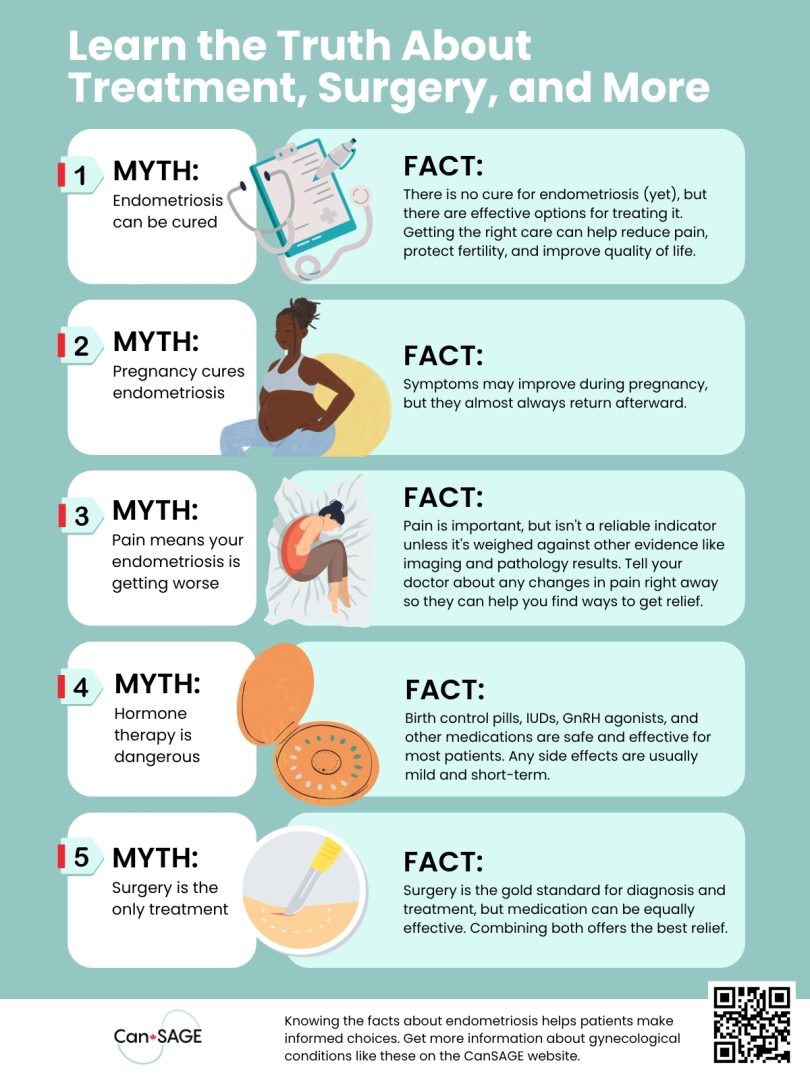
Below, you’ll learn the truth behind the top five endometriosis myths found online, including whether hormone therapy is really dangerous, if pregnancy will cure your endo, and how early referrals help.
The Top 5 Endometriosis Myths Busted
Misunderstandings about getting care or treating endometriosis can hold people back from getting the care they need. Myths like these are common on social media sites like Facebook, Instagram, and TikTok, but they often aren’t accurate and could even be hazardous to your health.
Here’s a look at some of the most common myths about endometriosis so you can separate fact from fiction.
1. [____] Will Cure Your Endometriosis
Status: FALSE.
There is currently no cure for endometriosis.
The Truth:
No food, health supplement, exercise, therapy, or procedure can cure your endometriosis completely, although this may change in the future. Treatments like hormone therapy and surgery can improve quality of life, preserve fertility, relieve pain, and protect nearby organs from harm but won’t cure it completely.
2. Pregnancy Will Cure Your Endometriosis
Status: FALSE.
Symptom relief during pregnancy is temporary, and pregnancy is not a cure.
The Truth:
Pregnancy raises progesterone levels, which suppresses ovulation and lowers estrogen activity in the body. While it’s true that some patients notice a temporary improvement in their symptoms while pregnant or breastfeeding, symptoms usually return to normal in the months or years after birth.
If your endometriosis improved during pregnancy, you may benefit from taking progesterone-only birth control pills or progestin-only pills (norethindrone, dienogest). They mimic similar changes in the body, but may not be as effective in patients with progesterone resistance.
3. Pain Proves Your Endometriosis is Getting Worse
Status: FALSE.
Pain is a subjective experience and isn’t always a reliable indicator of disease severity.
The Truth:
Pain is a common symptom of endometriosis. In fact, over 60% of patients struggle with it at some point, but no two people experience or cope with it in the same way. It’s just as common for someone with only a few lesions to report severe pain as it is for someone with many to report only mild discomfort.
Tell your doctor right away if your pain worsens or changes over time. They’ll weigh it against other evidence, like imaging and pathology reports, before deciding the best way to treat it.
4. Hormone Therapy is Dangerous
Status: FALSE (with a few caveats).
Hormone therapy is a safe and effective treatment option for most patients. But like any medication, it’s important to understand the risks and benefits of taking hormones.
The Truth:
Birth control pills, Intra-Uterine Devices (IUDs), Gonadotropin-releasing hormone (GnRH) agonists (like Lupron), and other hormone therapies can safely and effectively treat endometriosis. They work by suppressing ovulation and lowering estrogen activity in the body, both of which can cause lesions to grow.
There is a small risk (around 10 in every 10,000 people) of blood clots if you’re taking a pill that contains estrogen specifically. Your doctor will check for risk factors such as migraines, smoking, or personal history of clots before prescribing them.
IUDs, GnRH agonists, and progesterone-only medications don’t share the same risk profile. Side effects like nausea, headaches, and breast tenderness are typically mild and go away on their own. GnRH agonists can cause bone density loss over time, but they’re typically only used for short cycles.
5. Surgery is the Only Treatment for Endometriosis
Status: FALSE.
Surgery can be an effective method for removing lesions, but it isn’t the only treatment for endometriosis that exists.
The Truth:
Surgery is primarily used to diagnose endometriosis, to remove lesions that cause pain, or when nearby structures are at risk because of them. For example, you might have surgery to remove tissue on or near the bowel, bladder, and rectum. Sometimes, surgery may also improve your chances of fertility.
Read More: Endometriosis and Fertility: What You Need to Know
Hormone therapies and medications won’t remove lesions or improve fertility rates, but they can be just as effective at controlling painful symptoms. Patients who combined surgery with hormone therapy in clinical trials got even better results than they would by using only one or the other.
Why Early Referral is So Essential
Getting referred as early as possible gives you a head start when wait times are high, which is currently the case in most of Canada. If it takes two years to see a specialist, getting on the list now is still faster than waiting another year before you ask your doctor to put the referral in.
It also raises the chance for you to get a diagnosis and start first-line treatments, like hormone therapies, before your endometriosis becomes more severe. There is evidence to suggest that even a tentative diagnosis and treatment can help slow the progression of the disease over time.
Feeling better for a while, no matter what the cause is, isn’t a sign that you no longer need a referral or shouldn’t be followed by a specialist. You’ll still need a long-term care plan even if it consists of regular check-ins to make sure it isn’t getting worse again.
Finding Accurate Info About Endometriosis Matters
Patients and professionals should stay informed about endometriosis and know how to find accurate, up to date information about hormone therapies, surgery, and other treatments. Just taking a few minutes to question what you read, confirm if it’s based on real evidence, or talk it over with your doctor can help you avoid misconceptions and myths that do more harm than good.
For more endometriosis resources, visit CanSAGE’s videos page.