Summary:
Endometriosis can complicate fertility, but it does not make pregnancy impossible. Myths about infertility, pregnancy as a “cure,” or the lack of minimally invasive options often obscure the facts. In reality, many people with endometriosis conceive naturally or with medical, surgical, or assisted reproductive support. Surgical techniques like laparoscopy, excision, or ablation are minimally invasive and can improve fertility outcomes, especially in milder cases.
Endometriosis and Fertility: What You Need to Know
In addition to the physical pain it often causes, endometriosis is often associated with fertility problems. However, having endometriosis does not necessarily mean you will become infertile.
Misinformation about endometriosis is still common, so it’s important to separate the myths from the facts regarding this condition and how it can affect your ability to become pregnant. We’ve created this guide as a helpful reference you can use to stay informed about the realities of endometriosis and fertility. Use it to educate yourself and have productive discussions with your healthcare providers about how to manage this condition if it affects you or one of your loved ones.
Understanding Endometriosis and Fertility
Endometriosis occurs when the functional tissue that normally lines the uterus exists outside the uterine cavity. This frequently causes pain, although 20-25% of patients with endometriosis experience no symptoms at all.
But pain is not the only way endometriosis can impact your quality of life. This condition also tends to cause chronic inflammation, scar tissue, and adhesions (scar tissue that forms between surfaces inside the body and causes them to stick together). It can also impact the way your ovaries function.
All of these symptoms can alter the anatomy of your pelvis. This can cause significant pain, including pain during menstruation (dysmenorrhea) and pain during or near sexual intercourse (dyspareunia).
You can learn more by watching this explainer video on endometriosis and deep dyspareunia below:
None of these things are guaranteed to cause infertility, and the exact methods by which endometriosis leads to infertility are still not well understood. However, any of the following factors can play a major role:
- The pain and inflammation endometriosis causes
- The adhesions or changes to your pelvic anatomy
- Disruptions to the way your ovaries function
- Changes to how receptive your endometrial tissue is
It is also critical to understand that infertility is not an inevitable consequence of being diagnosed with endometriosis. Many people with this condition are still able to conceive naturally or with assistance.
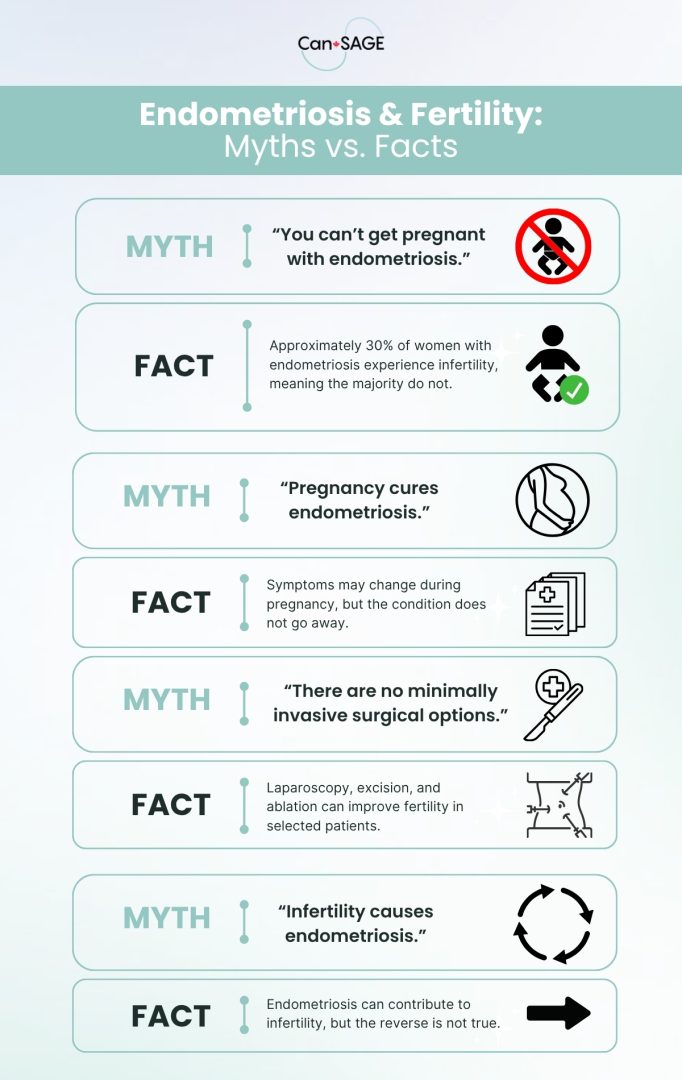
Common Myths About Endometriosis & Fertility
Some of the more common myths surrounding endometriosis and infertility include the following:
Myth 1: “If you have endometriosis, you can’t get pregnant.”
While endometriosis can make conception more difficult, most women with the condition are still able to become pregnant. Approximately 30% of women with endometriosis experience infertility, meaning the majority do not.
Endometriosis can interfere with fertility through impaired follicle development, lower egg quality, altered luteal function, and reduced fertilization or implantation rates. However, both natural and assisted conceptions still occur. Additionally, it is important to note that no additional pregnancy monitoring is recommended for women with endometriosis once conception happens, which suggests that successful pregnancy is common even when the condition is present.
Myth 2: “Pregnancy cures endometriosis.”
Some people diagnosed with endometriosis may be told that becoming pregnant can help mitigate their symptoms or stop the condition from getting worse. However, there has been no consistent association between getting pregnant and improvements in endometriosis symptoms.
Myth 3: “There are no minimally invasive surgery options for improving fertility with endometriosis”
Several minimally-invasive surgical techniques are commonly used to treat endometriosis, and some of these may also help improve fertility. Examples include:
- Laparascopy: This surgical method involves using a thin tube attached to a camera, as well as long surgical instruments to operate on endometrial tissue. Laparoscopic surgery can sometimes improve fertility outcomes and increase the likelihood of spontaneous conception.
- Excision or ablation: Excision is the process of cutting out the endometrial tissue that has grown outside of the uterine cavity, while ablation involves burning or vaporizing it. Both of these methods have been shown to increase pregnancy rates, although this data is only conclusive for patients with mild or minimal pelvic endometriosis.
However, it’s important to understand that all surgeries have limitations, and that surgery is not appropriate for everyone. If you believe that you have endometriosis, talk to your healthcare provider. They may be able to refer you to a specialist who can help you evaluate your options.
You can learn more about surgical approaches to treating endometriosis by watching the video below:
Myth 4: “Infertility causes endometriosis.”
Infertility does not cause endometriosis, although endometriosis does sometimes cause infertility. Ovarian endometriosis (which occurs when endometrial tissue grows on or inside the ovaries) can reduce the ovarian reserve, particularly in more severe cases. However, this also naturally occurs with age. And although endometriosis is more common in women in their 30s or 40s, it isn’t as common after menopause. In fact, many people diagnosed with endometriosis after menopause probably had endometriosis beforehand and just didn’t know it.
Fertility Options & Family Planning Pathways
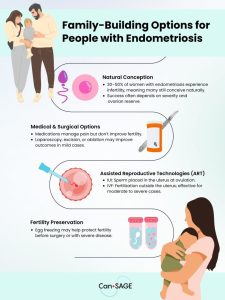
Natural Conception
For many people with endometriosis, natural conception is still possible. Only 30-50% of women with endometriosis experience infertility. Success rates largely depend on the severity of the disease. The more severe your endometriosis is, the more difficult it may be to conceive.
Medical & Surgical Options
There are several types of medications commonly used to treat endometriosis, but these will not make you more likely to become pregnant. They are either anti-inflammatories or medications that affect your hormones and temporarily stop the menstrual cycle.
As mentioned above, laparoscopy, excision, and ablation may all help improve fertility outcomes in some patients with minimal or mild endometriosis. In people who have a more severe case of endometriosis, having surgery may still improve the odds of becoming pregnant. However, these people may still have a lower likelihood of becoming pregnant than someone whose endometriosis is more mild.
Assisted Reproductive Technologies (ART)
Several techniques have been developed to assist with pregnancy using modern technology. Here are some that may be effective for improving fertility in people with endometriosis:
- Intrauterine insemination (IUI): This method involves placing a concentrated sperm sample into the uterus near the time of ovulation. IUI may be a viable option for improving fertility rates in cases where they have been impacted by endometriosis.
- In vitro fertilization (IVF): IVF remains an effective treatment option for many patients with endometriosis. This method involves fertilizing ovarian cells (oocytes) outside of the uterus.
Fertility Preservation
The process of egg freezing may make it easier to conceive via IVF later in life, due to the ovarian tissue damage that often occurs in severe endometriosis cases or after repeated surgeries.
Talking to Your Doctor
If you have questions about fertility and endometriosis, you should always discuss them with your healthcare provider. They can help you assess your options and create a plan of action that works for you.
When you approach your doctor, it can help to bring specific questions. Many patient advocacy organizations and clinical guidelines recommend asking questions like:
- What are my short- and long-term options for managing pain or other symptoms?
- I’ve heard about [X treatment option]. Do you think it’s appropriate for me? What are the pros and cons?
- Do you have recommendations for complementary care or educational resources?
- Can you refer me to a gynecologist with expertise in minimally invasive gynecologic surgery?
Note: Not all gynecologists are trained in excision surgery for endometriosis. If you have a specific surgeon in mind, you can request that your referral be sent directly to them.
Key Takeaways
Endometriosis and fertility are closely linked, but the relationship is far more nuanced than most common myths suggest. While some patients do experience difficulty conceiving, infertility is not inevitable, and a wide range of medical, surgical, and assisted reproductive options exist to support family planning.
The most important step is seeking accurate information and working closely with healthcare providers who can tailor recommendations to your individual situation. With the right guidance, many people with endometriosis are able to build the families they hope for.
Learn more about endometriosis by exploring our videos on this subject.