Summary:
Patients scheduled for laparoscopy for endometriosis may need to attend a Preoperative Clinic first. On surgery day, they’ll meet with the surgical team, change into a gown, and receive a general anesthetic through an IV. Once asleep, the surgeon will make small incisions in the abdomen, inflate it with gas, and use a laparoscope to complete the procedure. Recovery from laparoscopic surgery is rapid and typically is from 1-2 weeks but this can depend on the extent of the surgery.
What to Expect Before, During, and After Laparoscopy Surgery for Endometriosis
Laparoscopy can be an important part of treatment for endometriosis, along with medications and complementary strategies. For some patients, surgery is not required at all, but for others, surgery plays a critical role in addressing the disease for symptom relief and possibly to assist in fertility.
When to proceed to surgery, if it is necessary, and a clear delineation of the goals of surgery are important points to discuss with your surgeon before consenting to surgery.
Knowing what to expect before, during, and after your surgery is the best way to ensure your procedure goes smoothly. Below, you’ll learn what happens in each stage, how to prepare, and how long to expect recovery to take after you’re released.
Download the Laparoscopic Surgery for Endometriosis Prep Kit
Want an easy-to-follow, step-by-step guide to keep on hand? CanSAGE’s Laparoscopic Surgery for Endometriosis Prep Kit is free to access and easy to download or print off:
- Click the button below to download the PDF file
- Save it as a PDF on any compatible device for digital access
- Print it off to create a paper copy you can fill out and/or bring to the appointment
- Use the checklist as a quick reference on what to bring and how to get ready
- Add your own notes in the blank sections at the end of the checklist
Download the Laparoscopic Surgery for Endometriosis Prep Kit PDF
Before Your Surgery
The surgical process starts with an appointment with your surgeon, who will explain why surgery is recommended and clearly outline what will be done during the surgery (goals of surgery). They’ll also give you time to ask about the risks and benefits.
Common questions include:
- How long will my surgery take?
- Can you explain how you’ll remove or treat my endometriosis lesions?
- Will you examine my uterus, ovaries, and fallopian tubes during the procedure?
- What are the risks or possible complications associated with my surgery?
- What’s the best way to manage my pain before and after?
- What medications will you prescribe, and how should I take them?
- How much time should I plan to take off from work or school?
- Will I have restrictions during recovery (lifting, exercise, sex, driving)?
- When should I schedule a follow-up appointment?
- Will my symptoms improve after surgery, and if so, how much?
- What if I need another surgery in the future?
Some patients find it helpful to bring a notebook and a pen, a support person, or a phone to record the answers and take down details during the appointment.
Finding Out Your Surgery Date
Most patients find out the date of their surgery weeks or months in advance, but you might be placed on a cancellation list and get short notice instead. Once a date is set, the hospital will contact you for further instructions.
Pre-Operative/Pre-Admission Clinic
You may be required to attend a Preoperative/Pre-Admission Clinic, depending on whether you have other medical or anesthetic considerations before your surgery. This clinic may be called a different name depending on where you live.
At the Preop Clinic, you may speak to a nurse, an Internal Medicine Specialist, and/or an Anesthetist to ensure that all aspects of your medical history are covered.
Their job is to:
- Go over your full medical history with you, including all diagnosed conditions.
- Ask about allergies to medications, anesthesia, latex, and other common materials.
- Review your medications, including any prescriptions, OTC drugs, and supplements.
- Explain the anesthesia process and any post-operative pain management strategies.
- Schedule you for routine tests, like bloodwork, urine samples, or electrocardiograms (ECGs).
Let the team know if you have any illnesses, infections, bleeding disorders, auto-immune diseases, or a history of poor reactions to anesthesia (e.g., malignant hyperthermia). It is important to be up front about this information to ensure that your surgery is safe and effective.
Pre-Op Instructions From Your Doctor
The surgeon’s office and/or the hospital will contact you prior to your surgery, even if you have attended the Pre-Admission/Pre-Operative Clinic. They will provide you with all the details regarding getting ready for your surgery date. You will receive instructions regarding the following:
- If you need to stop using alcohol, cannabis, or medications (like semaglutide).
- When to stop NSAIDs, like naproxen, ibuprofen, or aspirin, to reduce bleeding risks.
- Have pre-surgical bloodwork, imaging, a pregnancy test, or a COVID test.
- Quit smoking or switch to a safer smoking alternative, like a nicotine patch.
- When to stop eating and drinking (this is typically at least 6-12 hours before your surgery, but the hospital will give you specific instructions based on their protocol)
- If you need to clean your skin with special soap or antibacterial wipes the night before.
The instructions you get might be different depending on your overall health or the specifics of your procedure. Ask your doctor for clarification if anything isn’t clear.
What to Pack in Your Hospital Bag
Having what you need while you’re at the hospital can help make recovery more comfortable and less stressful. Start with the items on this checklist, but pack light unless you’re being admitted afterward.
- Loose-fitting clothing and underwear (nothing tight at the waist).
- Overnight-style menstrual pads or period underwear (no tampons).
- Phone and charger with a long cord.
- Headphones or earbuds and a charger with a long cord.
- Comfort items (books, sweaters, blankets, pillows).
- Toiletries (toothbrush, lip balm, moisturizer, hair ties, face wipes).
- Glasses, contacts, contact solution, and storage case.
- Health card, ID, and hospital paperwork.
- All OTC and prescription medications.
- Non-perishable snacks (crackers, trail mix, granola bars).
- A reusable water bottle or thermos.
On The Day of Your Surgery
You’ll arrive at the hospital a few hours before the surgery and head to the surgical admissions desk first to check in. Someone will confirm your identity and walk you through any paperwork, then show you to the waiting area to follow these next steps.
1. Change Into a Hospital Gown
A nurse will take you to a dressing room where you’ll be asked to remove all jewelry, piercings, and nail polish and change into a gown. You may be asked to put on compression stockings, too.
2. Vitals Check
The nurse will check your vitals, including heart rate, blood pressure, and oxygenation rate.
3. IV Placement
Next, they’ll place an IV into your arm or hand. They might hang IV fluids or give you medications for anxiety before you head to the operating room.
4. Going to the OR
Once the team is ready, you’ll be wheeled down to the OR in a stretcher. The surgeon and anesthesiologist will stop to ask a few final questions before you go in.
5. Oxygenating Your Lungs
Someone will place an oxygen mask over your face. It might feel strange at first or difficult to take a deep breath—some patients describe it as being “denser” or “thicker” than normal air.
6. Sedation/Anesthesia
The anesthesiologist will give you medication to put you to sleep through your IV. They will guide you calmly as you drift off to sleep.
7. Performing the Laparoscopy
Once you’re asleep, the surgeon will make a series of small cuts on your abdomen and inflate it with gas so they can see more clearly. They’ll insert a thin tube with a camera (laparoscope) and tools, then use it to assess, remove, biopsy, or destroy any lesions.
8. Closing Up
The last step is to release the gas from your abdomen and stitch up any incisions. Your surgeon might use stitch material, glue, or steri-strips to keep them closed and in place.
9. In the Recovery Room
You’ll wake up in the recovery room and be closely monitored for the first 30-45 minutes. A nurse will check your vitals and give you medication to control your pain.
10. Going to a Room or Going Home
Most laparoscopic procedures are day procedures meaning that you get to go home the same day. If you have problems with voiding or with ongoing pain, or if there are concerns regarding your recovery, you may be admitted overnight for observation. Ensure that you have someone to drive you home and to stay with you for 1-2 days to act as support as you recover.
Tip: Hospitals won’t typically release patients the same day unless they have a support person who can stay with them for the first 24 to 48 hours. Don’t try to drive or operate heavy machinery.
What to Expect During the Recovery Process
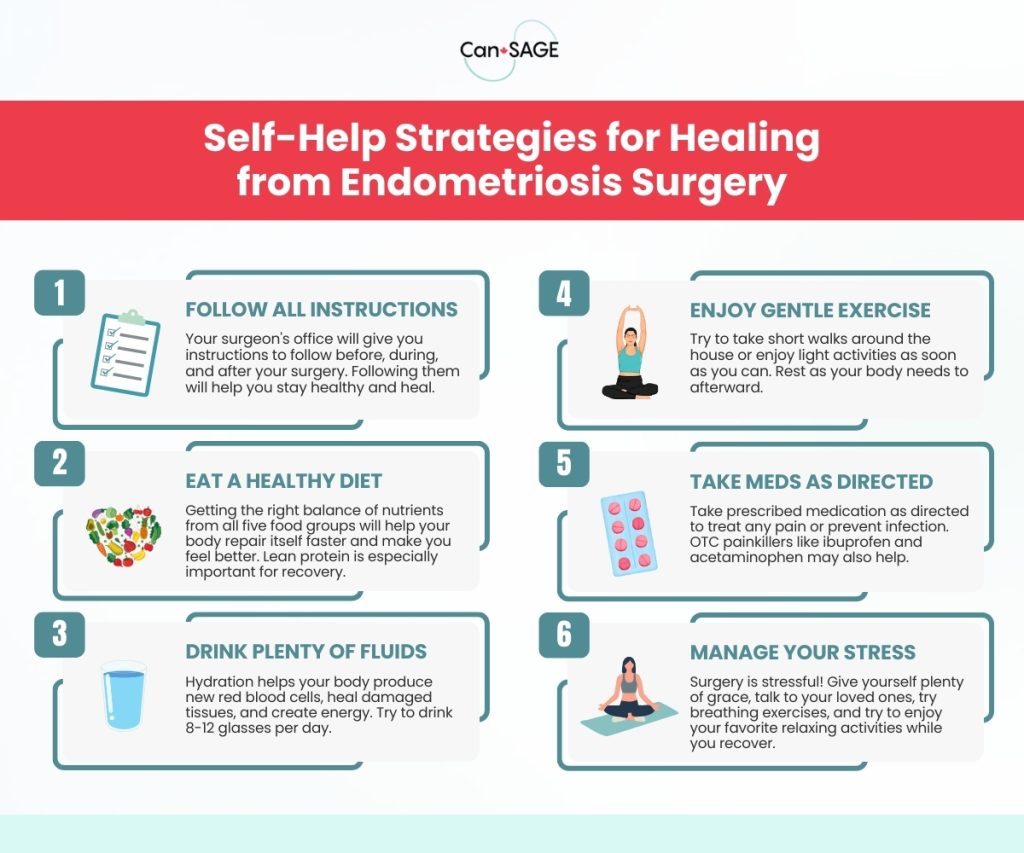
The biggest benefit of laparoscopic surgery is that it’s minimally invasive. That means patients recover faster than people who have open surgeries and can usually return to their normal activities sooner. You’ll still need to take time off to heal.
Recovering from laparoscopy happens in stages:
- The First 24–48 Hours: You’ll feel groggy from anesthesia and your incision sites may feel sore or achy. Some patients feel nauseous or experience shoulder and chest pain from the gas.
- Week 1: You may tire easily or notice bloating, cramping, or light vaginal spotting. Short walks around the house and light activities can help you recover faster, but you’ll need frequent rest.
- Week 2: Most people go back to work at this point with a gradual introduction of usual activities (like exercise) at this point.
Your recovery period might be longer if you have more incisions or your surgeon needs to switch to an open surgery called laparotomy (this is extremely rare).
When To Call the Doctor
Only around 0.4% to 3% of patients experience complications after laparoscopic surgery for endometriosis. Most are minor and don’t affect the outcome.
If you are going to the ER for a serious complication, make sure to let your surgeon’s office know that you attended an emergency room. If you experience a minor complication, such as an infected incision or a possible urinary tract infection, this can be dealt with in the office. Reach out to your surgeon or a family doctor to be seen ASAP.
Call the surgeon right away if you experience:
- Fever above 38°C (100.4°F).
- Confusion, delirium, or difficulty staying awake.
- Heavy vaginal bleeding (soaking through a pad in 1-2 hours).
- Severe abdominal pain that isn’t controlled with medication.
- Redness, pus, swelling, or discharge around the incision sites.
- Difficulty breathing, chest pain, or persistent nausea/vomiting.
Remember: if you’re ever uncertain about whether something is normal, it’s safer to call the office or head to your local emergency room instead of trying to wait it out.
Make the Most of Your Laparoscopy for Endometriosis
It’s easy to assume the surgeon is the only one who has the power to impact surgical outcomes. Their skill and experience do make a difference, but it’s even more important for you to be an active participant in the process. Ask questions, follow all instructions carefully, and let yourself rest when you feel like you need it—it’s the best way to ensure a positive outcome that delivers real relief.
Learn more about endometriosis: explore our Endometriosis videos page.