Your first Pelvic Floor Physical Therapy appointment can be a little daunting. Pelvic health expert Stephanie Prendergast is here to help you understand what to expect during your first PT session and ease any worries you may have.
Pelvic Pain Management Explained
Chronic pelvic pain can have many causes, including endometriosis, vulvodynia, interstitial cystitis, irritable bowel syndrome, or musculoskeletal issues. Managing this pain often requires a holistic approach that combines medical treatment with physical therapy, lifestyle changes, and psychological support.
Our pain management video library helps you understand pelvic pain, what therapies are available, and how to use tools like breathing, stretching, and mindfulness to improve quality of life.
These videos and resources are recommended by Canadian doctors and international pain specialists.
Pelvic Pain Management FAQs
What is pelvic floor physical therapy (PFPT) and how does it help with pain?
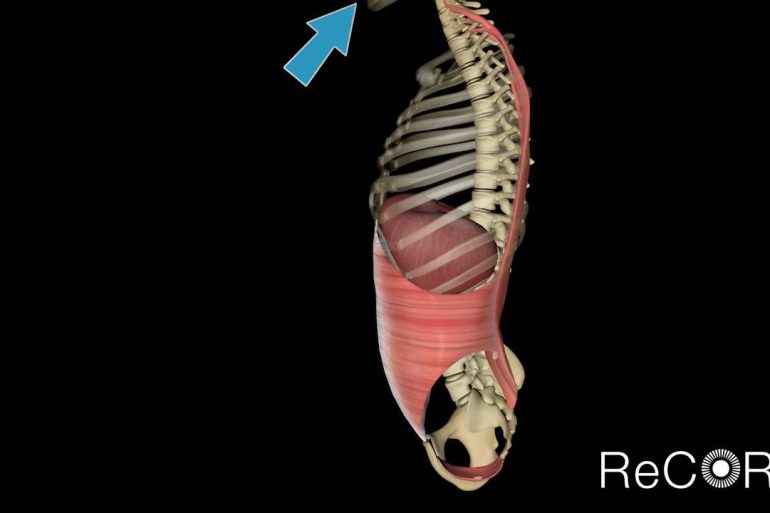
PFPT uses targeted exercises, stretches, and hands-on techniques to reduce pelvic pain, relax tight muscles, and improve mobility. Many patients find it reduces chronic discomfort and improves daily function.
Are there at-home strategies to manage pelvic pain?
Yes. Techniques like diaphragmatic breathing, posture awareness, and gentle stretches (such as child’s pose or cat-cow) can help relax the pelvic floor and reduce tension. Online guided videos are also widely available.
Can chronic pelvic pain be linked to mental health?
Chronic pain often affects both body and mind. Anxiety and stress can heighten pain sensitivity, while depression may worsen symptoms. Apps like Curable or programs like PainTrainer offer psychological tools for coping and recovery.
Where can I find a pelvic floor physical therapist?
Directories such as pelvicrehab.com, Pelvic Pain.org, and Pelvic Guru can connect you to trained therapists. Many now offer virtual consultations.
What role does exercise play in managing pain?
Gentle mobility, stretching, and strengthening can improve posture and reduce pain. Foam rollers, small balls, or yoga poses are often incorporated for self-release and flexibility.
Where can I find resources for condition-specific pelvic pain?
Several dedicated organizations provide education and support:
Endometriosis: SWHR Toolkit
Vulvodynia: National Vulvodynia Association
Interstitial Cystitis: IC Association
IBS: About IBS
Can lifestyle changes make a difference?
Diet, stress management, and sleep routines can all impact chronic pain. Free handouts like Managing Chronic Pelvic Pain Through Diet and mindfulness-based practices can be used to support long-term improvements
What are some trusted psychology-based pain programs?
Options include:
Curable App: Neuroscience-based education and tools
Pathways App: CBT, mindfulness, and meditation
Tame the Beast: Animated education on how chronic pain works
PainTrainer: Free online program with coping strategies
Additional Pelvic Pain Resources
To locate a trained pelvic floor physical therapist:
https://ptl.womenshealthapta.org/
https://www.pelvicpain.org/public
Many offer Virtual Consultation and 1:1 Virtual Therapy, others offer paid memberships:
https://pelvicguru.com/directory/
https://beyondbasicsphysicaltherapy.com/pages/our-services
Power Over Pain Portal
Get support. Get Empowered. The Power Over Pain Portal is your ultimate online resource for comprehensive pain management. We offer interactive courses, education, tools, peer support and workshops to support your pain management journey.
Free
Pelvic Rehabilitation: Retrain Your Pelvic Pain
https://www.pelvicrehabilitation.com/retrain-your-pelvic-pain/
6 week online program taught by Dr. Alexandra Milspaw reviewing the neurobiology of pain, mindfulness-based cognitive techniques, and neuro-linguistic programming techniques aimed at reducing pain and increasing resiliency
$300
PainTrainer
www.paintrainer.org
Online program which teaches effective strategies to manage pain over 8 sessions
Free
Chronic pelvic pain overview:
‐International Pelvic Pain Society (IPPS): https://www.pelvicpain.org/public/resources/educational‐resources/informational‐handouts
‐Pelvic Pain Education Program: https://www.pelvicpain.org/public/resources/educational‐resources/informational‐handouts
Endometriosis:
‐Society for Women’s Health Research: https://swhr.org/wp-content/uploads/2021/03/SWHREndometriosisToolkit_3.2021.pdf?msclkid=453652b3d15011ec97b4d08a18998416
‐Endometriosis.net: https://endometriosis.net/
Vulvodynia:
‐National Vulvodynia Association: https://www.nva.org/
‐Vulval Pain Society: https://vulvalpainsociety.org/
Pelvic myofascial pain:
‐Beyond Basics Physical Therapy: https://beyondbasicsphysicaltherapy.com/pages/books‐and‐products
‐Pelvic Health and Rehabilitation Center: https://pelvicpainrehab.com/
YouTube: https://www.youtube.com/channel/UCKIfy8‐P10EyTaM‐bIbeFbA
Interstitial Cystitis/Bladder Pain Syndrome:
‐Interstitial Cystitis Association: https://www.ichelp.org/
YouTube: https://www.youtube.com/user/ICHelp
Irritable Bowel Syndrome:
‐International Federation for Gastrointestinal Disorders: https://aboutibs.org/
‐UNC Center for Functional GI & Motility Disorders: https://www.med.unc.edu/ibs/patient‐education/educational‐gi‐handouts/
Nociplastic pain:
‐PainGuide: https://painguide.com/
‐Tame the Beast: https://www.tamethebeast.org/
‐Understanding Pain in less than five minutes: https://www.youtube.com/watch?v=5KrUL8tOaQs
Additional:
BC Women’s Centre for Pelvic Pain and Endometriosis
International Pelvic Pain Society (IPPS)
International Association for the Study of Pain (IASP)
National Vulvodynia Association (NVA)
Calgary Chronic Pain Centre
Alberta Healthy Living Program
University of Michigan FibroGuide (https://fibroguide.med.umich.edu/pain- care/self-care/)
Pelvic Pain Support Network https://www.pelvicpain.org.uk/
Pain BC