Summary:
Endometriosis affects about 1 in 10 women and often causes pain in the pelvis, back, hips, legs, bladder, or bowels. High estrogen levels, poor sleep, diet, stress, and other factors can trigger flare-ups that make symptoms worse. Common coping strategies include heat, gentle movement, and anti-inflammatory foods, but if these aren’t enough, your doctor might recommend hormone therapies, birth control pills, an IUD, a TENS machine, or surgery instead.
Understanding Endometriosis Pain: Types, Triggers, and Coping Strategies
Endometriosis is a condition where tissue similar to the inner lining of your uterus (called the endometrium) starts to grow in other areas of the body. This tissue responds to changing hormone levels throughout your cycle, so it thickens, breaks down, and bleeds in the same way, but can’t exit the body.
Over 60% of the 1 in 10 women who are diagnosed with endometriosis struggle with chronic pelvic pain, but it isn’t always easy to recognize where it’s coming from at first. It can move around, mimic bowel and bladder problems, or even feel like it’s coming from your back or legs instead.
In this guide, you’ll learn about the different types of endometriosis pain, how it might affect you, and what makes it worse. We’ll also share evidence-based strategies that might help you cope.
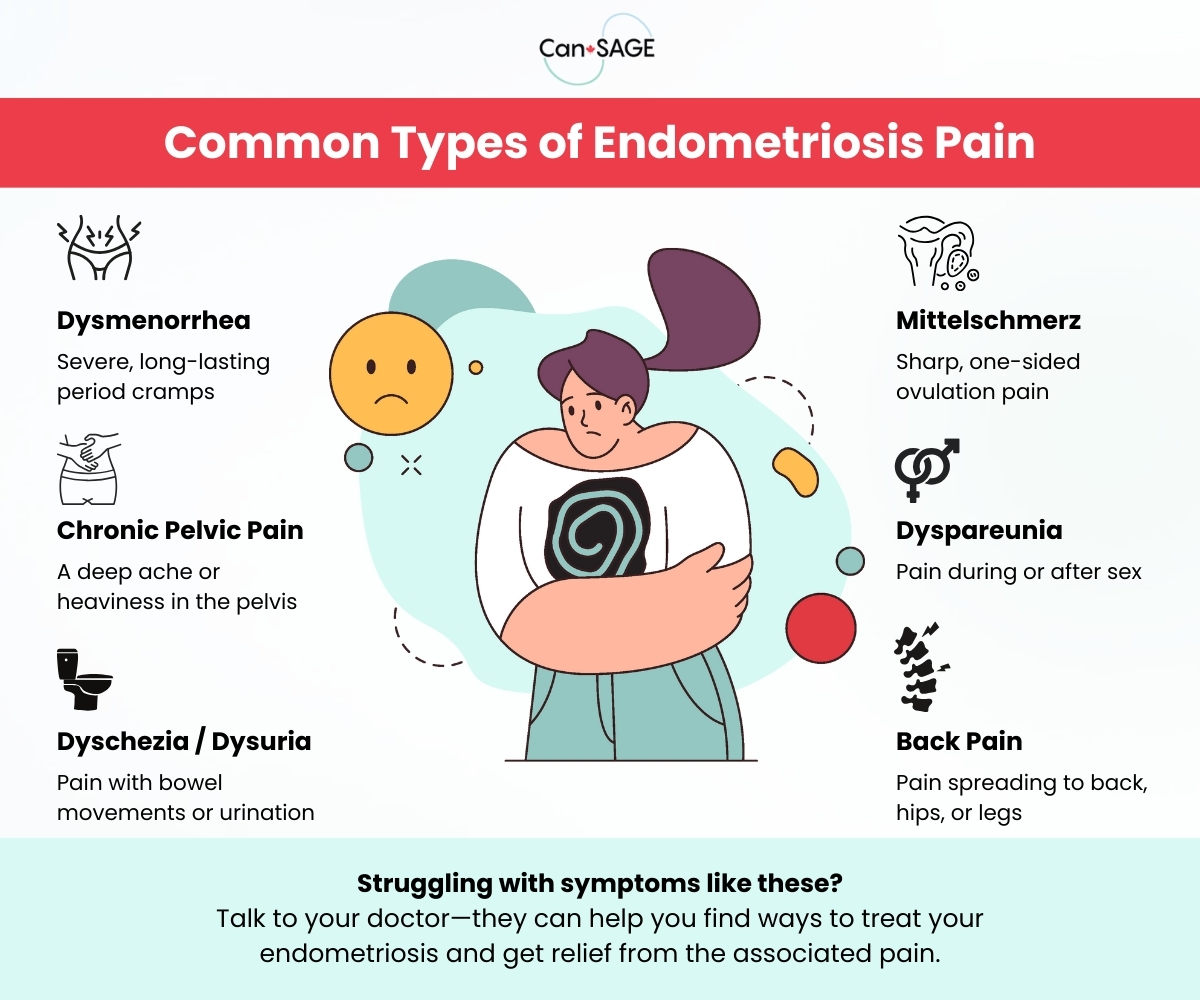
Types of Endometriosis Pain
Endometriosis pain doesn’t always look the same for every patient. The intensity and location can change day-to-day and depend on factors like:
- Where your lesions form
- How big they are
- Whether they put pressure on nearby nerves
Your pain will usually fall into one of a few known categories:
Pain During Your Period
Severe discomfort and cramping during periods is so common in endometriosis that it’s often what drives people to seek help for their symptoms in the first place.
- Common Medical Terms: Dysmenorrhea
- How Patients Might Describe It: “Cramping that knocks me out for days,” “Painkillers don’t even touch it,” or “It feels like early labor contractions.”
What Causes It?
Lesions that grow outside of the uterus release hormones called prostaglandins that trigger inflammation locally. They make your uterus contract harder and more often during your period, causing cramps to feel stronger and last longer than they normally would.
Pain in Your Pelvis or Lower Abdomen
Endometriosis can cause a deep, constant ache or discomfort that’s always present, regardless of whether you’re on your period.
- Common Medical Terms: Chronic Pelvic Pain (CPP)
- How Patients Describe It: “A heaviness in my pelvis all the time,” “An ache that feels like pressure or dragging,” or “It feels like my muscles are being stretched.”
What Causes It?
Swelling and scar tissue from endometriosis puts pressure on the nerves throughout your lower stomach. It also encourages tiny new nerve endings to grow into and from the lesions themselves. With more nerves picking up signals, your pelvis is more likely to feel sore or sensitive all month long.
Pain During Ovulation
Some endometriosis patients experience a short, sharp pain on one side of the pelvis around the halfway point of their cycle and/or when they ovulate.
- Common Medical Terms: Mittelschmerz
- How Patients Describe It: “A sudden jab on one side,” “Like being poked with a knife in my ovary,” or “An electric shock that takes my breath away.”
What Causes It?
Ovulation pain isn’t exactly rare, but it can be worse for patients with endometriosis. This is especially true if you have lesions near your ovaries or fallopian tubes.
Pain During Sex
Discomfort during sex, especially with deep penetration, is common in patients with endometriosis. It can be severe enough to prevent you from enjoying intimacy and close relationships with sexual partners.
- Common Medical Terms: Dyspareunia
- How Patients Describe It: “It’s a sharp pain like hitting a wall,” “A deep ache that lasts hours afterward,” or “Having sex hurts every time, even when we go slow.”
What Causes It?
Dyspareunia is strongly linked to lesions that develop on or near the uterus, cervix, or vaginal wall and/or the tissue separating the vagina and rectum. You may also struggle with bowel or bladder symptoms.
Pain When Using the Bathroom
Endometriosis can make it harder to pass stool and urine, cause pain when you go to the bathroom, or even cause you to pass small amounts of blood when you go.
- Common Medical Terms: Dyschezia (painful bowel movements), Dysuria (painful urination)
- How Patients Describe It: “It feels like I’m passing glass when I go to the bathroom,” “It burns every time I pee,” or “I think I might have a urinary tract infection (UTI).”
What Causes It?
Endometriosis lesions that develop deep in the pelvis or alongside nearby organs can cause bowel pain, constipation, or rectal bleeding, especially around your period. Urinary endometriosis typically involves the bladder and can sometimes present like a urinary tract or yeast infection.
Pain in Your Back, Hips, or Legs
In some cases, endometriosis can put pressure on nerve bundles that connect to the lower back, hips, or legs, causing a burning, stinging, or aching pain in those areas.
- Common Medical Terms: Neuralgia, Sciatica, Sciatic Endometriosis
- How Patients Describe It: “Pain shoots down my left/right leg every cycle,” “It feels like sciatica that gets worse with my period,” or “My lower back aches constantly during my period.”
What Causes It?
It isn’t always clear why this happens, but there is some evidence to suggest that it might be related to endometriosis lesions putting pressure on nerves deep within the pelvis. Sciatica that only seems to flare up during your period is one of the most common red flags.
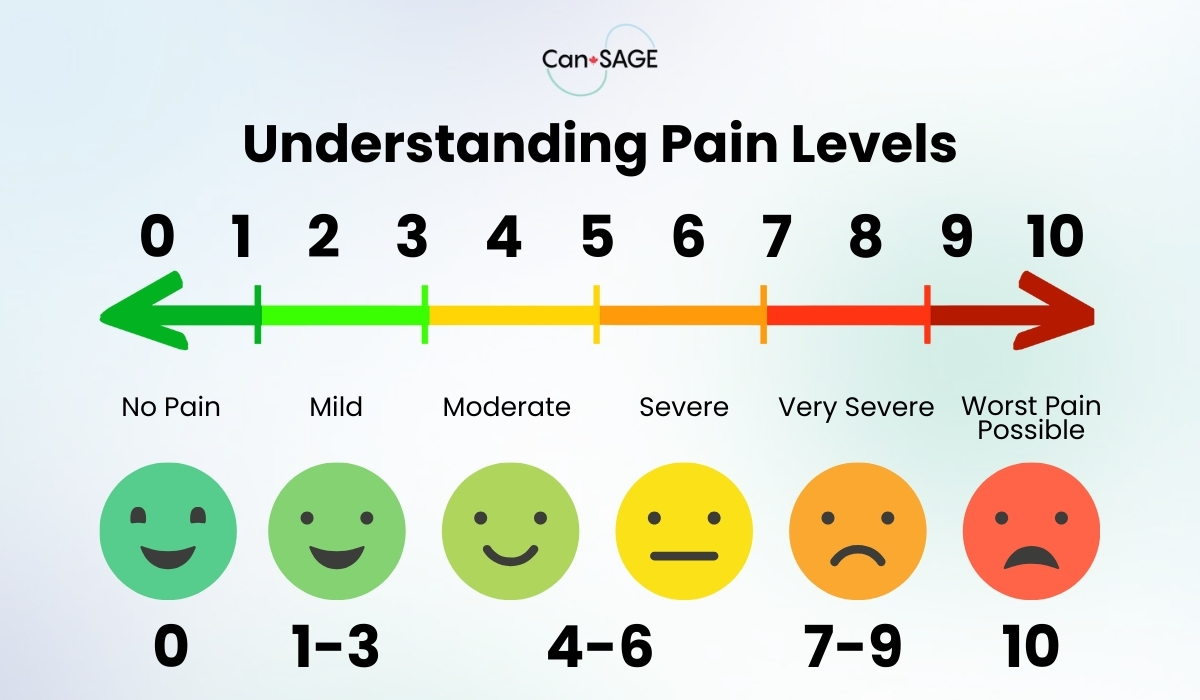
Describing Your Pain Accurately
If you struggle to put your symptoms in words when you see your doctor, you aren’t alone. Endometriosis symptoms are notoriously vague, and differences in the ability to cope means that what one person considers “severe” can be another person’s “normal.”
Try sharing details like these to help your doctor better understand what you’re going through:
- Descriptors: Use words like throbbing, stabbing, burning, cramping, dull, or stinging to help outline the pain. Include how it makes you feel physically and emotionally, too: fearful, anxious, exhausted, frustrated, or nauseous.
- Timing: Note when the discomfort happens: while you’re on your period, when you ovulate, when you have sex, or all the time. Keep a diary of your symptoms if you have trouble keeping track.
- Location: Be specific about where you feel it, if it stays in one spot, or if it spreads around to other areas of your body. Some patients find it helpful to color in a chart of the body.
- Severity: Rate your pain on a 0–10 scale when it happens, with 1 being no pain at all and 10 being the worst pain you’ve ever experienced.
- Impact: Share how the discomfort affects your quality of life. Does it make you miss work, cancel social plans, or delay meetings? Do you have days where you need to stay at home to cope?
Be sure to mention all types of discomfort you experience throughout the month, even if they don’t seem related to your endometriosis (like headaches). Even small details can help your doctor spot important patterns or track the progression of your condition.
Triggers That Worsen Endometriosis Pain
While we don’t yet fully understand the root causes of endometriosis, we do have strong evidence that suggests certain triggers make it worse. All of the following can lead to flare-ups that worsen your symptoms or make your condition worse:
- High Estrogen: Endometriosis is estrogen-dependent, so if you naturally have very high levels or experience spikes throughout the month it may make your symptoms worse. Lesions can also release estrogen themselves, which perpetuates the cycle.
- Inflammatory Foods: Diets that are very high in processed foods, dairy, caffeine, and gluten are linked to high levels of inflammation in the body. According to one 2025 study, between 45% and 53% of participants felt better after cutting them out.
- Stress: Higher stress levels increase the level of cortisol (a stress hormone) in the body. According to a 2024 study, this may intensify pelvic pain and cramping for patients with endometriosis.
- Poor Sleep: People with endometriosis who sleep poorly tend to experience more bladder discomfort, a lower quality of life, and more symptoms of depression. Your doctor can help you manage symptoms like insomnia or pain at night so you can get more rest.
- Not Getting Enough Exercise: It’s hard to stay active when you’re in a flare, but there’s evidence to suggest that gentle exercise improves quality of life for people with endometriosis.
- Digestive Changes: Bloating, constipation, and IBS-like symptoms often occur alongside endometriosis (or in addition to it). They can create a negative feedback loop that worsen flares and makes your pain worse throughout the month.
Identifying which of these triggers apply to you can help you find ways to limit their influence over your endometriosis and manage it more effectively.
Medical Pain Management Strategies
For many patients, simple at-home coping strategies aren’t enough to sufficiently manage their pain. If what you’re trying on your own at home isn’t working, it may be time to ask your doctor about medical pain management strategies like these:
- OTC Medications: Over-the-counter non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can help manage both pain and inflammation. Acetaminophen (Tylenol) only relieves pain, but is still worth trying—especially if you can’t take NSAIDs.
- Prescription Pain Control: Prescription-strength NSAIDs (Toradol, Diclofenac) and other pain medications (Cymbalta, Tramadol) may be an option for some patients. They’re typically only indicated for short-term use during severe flares.
- Hormone Therapy: Birth control pills (Yaz, Tri-Cyclen), GnRH agonists (Lupron), progestins (norethindrone) and other hormone therapies are very effective at slowing the growth of endometriosis. They may also shrink existing lesions.
- TENS Units: A transcutaneous electrical nerve stimulation (TENS) unit works by delivering mild electrical pulses through the skin. This makes it harder for your nerves to send pain signals to the brain and tells your muscles to relax.
- Intra-Uterine Devices (IUDs): Some patients find hormone-containing (Mirena) or copper-only (Para-Gard) IUDs effective. Devices that contain levonorgestrel are particularly effective.
- Surgery: If medication isn’t enough, your doctor may recommend a type of surgery called laparoscopy that involves removing lesions or scar tissue through tiny incisions. Total or partial hysterectomy is also an option, but is usually considered a last resort.
- Pain Management: If you continue to experience debilitating pain, you may benefit from being referred to a pain or chronic disease management clinic.
Most patients do better when they’re treated and followed by a clinic or specialist who understands endometriosis. If wait times are long in your area, your regular doctor can still help you manage symptoms and connect you with the resources you need.
At-Home Coping Strategies
Most people find that combining medical care with simple, day-to-day strategies makes the biggest difference in their symptoms. It’s safe to try strategies like these on your own:
- Heat: Heating pads, warm baths, and Epsom salt soaks can help relax the muscles deep in the pelvis and relieve spasms or cramps.
- Gentle Movement: Yoga, stretching, and short walks can help improve circulation and reduce muscle stiffness. It can also help you manage your stress.
- Anti-Inflammatory Foods: Eating anti-inflammatory foods like leafy greens, fruits, whole grains, and omega-3 fatty acids (salmon, certain nuts) may help relieve your symptoms.
- Stress Management: Counseling, mindfulness practices, and breathing exercises reduce stress levels and give you more tools to cope with your pain.
- Support Groups: Connecting with others who understand what it’s like to have endometriosis in person or online can help you feel heard and understood..
Keep in mind that endometriosis can change over time. If what you’re doing now stops working, or you experience a sudden increase in pain or cramps, let your doctor know right away.
Help Is Available for Endometriosis Pain
Endometriosis pain is a complex and deeply personal experience for most patients, but getting to know your condition and how it affects you will make it easier to manage. One of the most important steps you can take right now is to start tracking your symptoms and your periods. Spotting the patterns that make your endometriosis unique is the best way to find the right treatment.
Want to learn more about endometriosis? Explore our collection of endometriosis videos.